Table Of Content
- Multiple primary endpoints
- Design and Conduct of Clinical Trials
- Designing studies with a strong foundation I: preliminary clinical data
- Clinical trial design during and beyond the pandemic: the I-SPY COVID trial
- The argument framework is a flexible approach to evidence in healthcare
- Clinical Trials Analysis, Monitoring, and Presentation
Difficult as it is to believe, analyses comparing survival of responders versus non-responders remains common despite wide-spread knowledge such analyses are subject to diverse biases [45]. As numbers of endpoints increases the numbers of ways to allocate the α across endpoints also increases. Although there is no perfect all-encompassing study design for each trial situation, an overarching algorithm is depicted in Tables Tables22 and and44. Warts can be self-resolving and hence the efficacy of immunotherapy as opposed to the self-resolution compromises the validity of the results. An alternative method for calculating the sample size is to identify a primary quantity to be estimated and then estimate it with acceptable precision.
Multiple primary endpoints
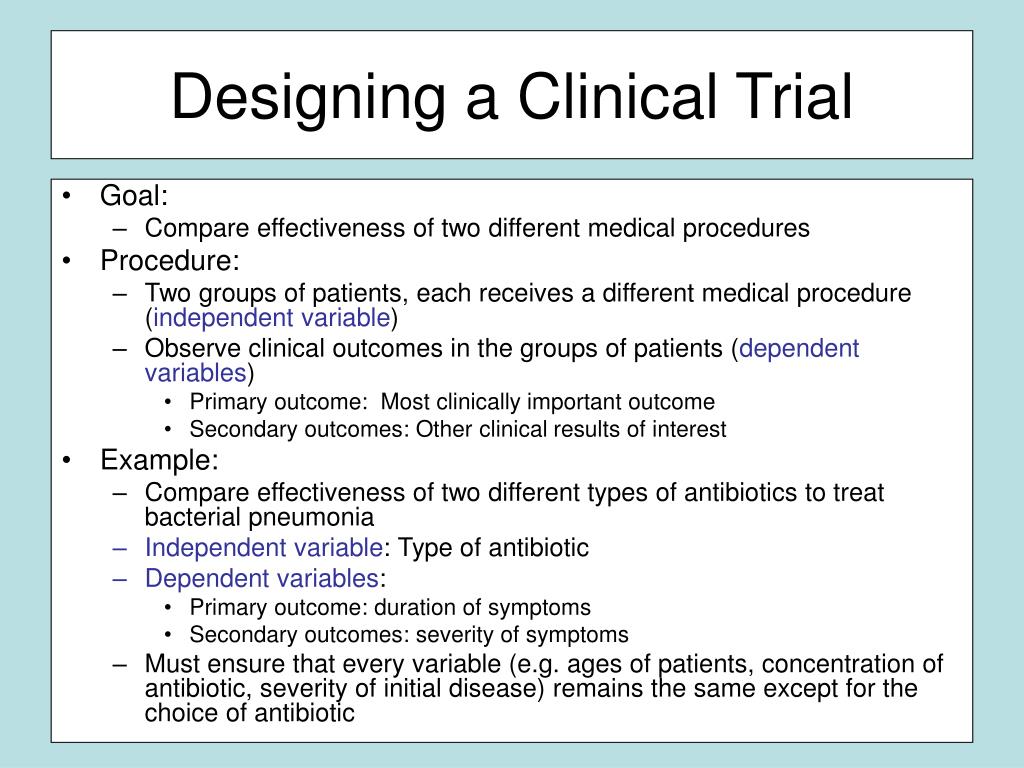
Clinical trials aim to advance science by deepening our understanding of the mechanisms of action and therapeutic effects of one or more interventions. However, the final purpose of most clinical trials is to gain regulatory approval of a specific agent, or to compare interventions within a target population (13). In conclusion, we hope that lessons learned from the I-SPY COVID trial will have important implications for the treatment of patients with severe COVID-19 and also for future trials in critically ill patients more generally. Third, studying a variety of agents across many months in a global pandemic has also highlighted the enormous advantages of platform trials that employ a concurrent control arm able to evolve with changes in the standard of care — a relatively unique feature of I-SPY COVID. The standard of care for severe COVID has shifted dramatically over the course of the pandemic, beginning with remdesivir in late spring 2020 and the addition of dexamethasone shortly thereafter.
Design and Conduct of Clinical Trials
It provides a way to avoid predicting which subjects are assigned to a certain group and therefore, prevent bias on the final results due to subject selection. This also ensures comparability between groups as most baseline characteristics are similar prior to randomization and therefore helps to interpret the results regarding the intervention/experiment group without bias. One of the limitations of case‐control studies is that they cannot estimate prevalence of a disease accurately as a proportion of cases and controls are studied at a time. Case‐control studies are also prone to biases such as recall bias, as the subjects are providing information based on their memory.
Designing studies with a strong foundation I: preliminary clinical data
Pain points: Unsolved recruitment and trial design issues in pain clinical trials - Clinical Trials Arena
Pain points: Unsolved recruitment and trial design issues in pain clinical trials.
Posted: Thu, 21 Sep 2023 07:00:00 GMT [source]
A staining cough drop could be given to study participants prior to evaluation to help maintain the blind. In late phase clinical trials, it is common to compare two active interventions. These interventions may have different treatment schedules (e.g., dosing frequencies), may be administered via different routes (e.g., oral vs. intravenously), or may look, taste, or smell different. A typical way to blind such a study is the “double-dummy” approach that utilizes two placebos, one for each intervention.
In order to conduct the appropriate analyses, specific data must be collected in a manner suitable to conduct the analyses. In order to collect these necessary data, a thorough plan for data collection must be developed. This sequential retrospective strategy continues until a trial design has been constructed to address the research question. In cross‐over clinical trial study design, there are two groups who undergoes the same intervention/experiment at different time periods of the study. That is, each group serves as a control while the other group is undergoing the intervention/experiment.14 Depending on the intervention/experiment, a ‘washout’ period is recommended. This would help eliminate residuals effects of the intervention/experiment when the experiment group transitions to be the control group.
Cohort study
In the first part of the course, students will be introduced to terminology used in clinical trials and the several common designs used for clinical trials, such as parallel and cross-over designs. We will also explain some of the mechanics of clinical trials, like randomization and blinding of treatment. In the second half of the course, we will explain how clinical trials are analyzed and interpreted.
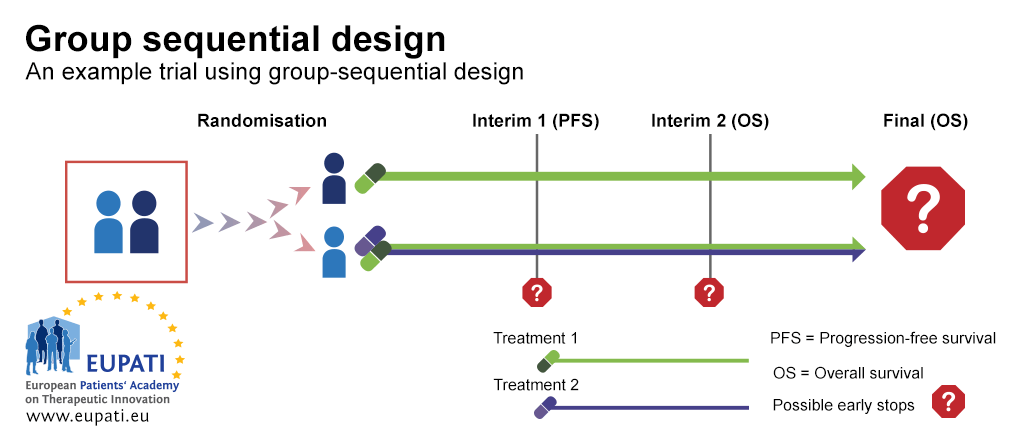
Although initially drawing from the existing I-SPY2 site network, the trial has expanded to more than 30 sites across the United States and has enrolled over 2,100 patients. The disadvantages of this design are (1) Missing data due to withdrawals that can be countered by imputation or using time to event analysis. (5) Not suitable for unpredictable diseases (e.g., spontaneous remission) or those with slow evolution; hence, can be used only for chronic stable diseases. In many situations, more than one efficacy endpoints are used to address the primary objective. Decisions regarding how the statistical error rates (e.g., Type I error) will be controlled should be described in the protocol and in the statistical analysis plan.
Thus trials investigating the effects of such interventions might employ stratified randomization based on gender. For example, two randomization schedules may be utilized; one for males and another for females. Stratified randomization ensures that the number of male participants in each treatment group is similar and that the number of female participants in each treatment group is similar. First, stratification can only be utilized for known and measurable confounders. Secondly, although one can stratify on multiple variables, one has to be wary of over-stratification (i.e., too many strata for the given sample size). The sample size must be large enough to enroll several participants for each treatment from each stratum.

Clinical Trials Analysis, Monitoring, and Presentation
Moreover, often a variety of manipulations are used to control for the false-positive rate across analyses. False-positive errors are further discussed below as different topics intersect with error control in clinical trials. In a conventional pilot study, participants are often ineligible for analysis along with cases in future definitive studies due to concerns about selection bias, carry-over, and training effects. Where patients are few in number as in case of rare diseases, allocating them to a pilot study rather than the definitive study could be seen as a wasteful approach.
This is important because each person on the team contributes their area of expertise to come up with a feasible study that meets the scientific hypothesis. It is crucial to involve statisticians in the very early stage of the study design instead of waiting to involve them at the time of data analysis. Note that it is very difficult to fix a poorly-designed study once it is implemented. Clinical trials are a fundamental component of medical research and serve as the main route to obtain evidence of the safety and efficacy of a treatment before its approval. A trial’s ability to provide the intended evidence hinges on appropriate design, from background knowledge and trial rationale to sample size and interim monitoring rules.
Blinding refers to keeping study participants, investigators, or assessors unaware of the assigned intervention so that this knowledge will not affect their behavior, noting that a change in behavior can be subtle, unnoticeable, and unintentional. When study participants are blinded, they may be less likely to have biased psychological or physical responses to intervention, less likely to use adjunct intervention, less likely to drop out of the study, and more likely to adhere to the intervention. Blinding of study participants is particularly important for patient reported outcomes (e.g., pain) since knowledge of treatment assignment could affect their response.
The primary objective of the trial is to address the scientific question by collecting appropriate data. The selection of the primary endpoint is made to address the primary objective of the trial. The primary end-point should be clinically relevant, interpretable, sensitive to the effects of intervention, practical and affordable to measure, and ideally can be measured in an unbiased manner. The larger the variation, the more difficult it is to identify treatment effects. One important method for reducing variation is to construct consistent and uniform endpoint definitions.
However, it helps to control the balance between the experiment/intervention groups. Clinical trials are further divided into randomized clinical trial, non‐randomized clinical trial, cross‐over clinical trial and factorial clinical trial. Each trial is conducted in stages, so it’s critical that you and your team are prepared to make sound design choices for each stage. That includes developing and evaluating research questions and hypotheses, selecting among various design types, and identifying errors.
When the disease is rare and/or a targeted subgroup is of interest, then specific study designs for these settings may need to be considered; see Le-Rademacher et al. (2018), Gupta et al. (2011), and Mandrekar and Sargent (2009). Similarly, there is extensive work in the literature on study designs for personalized medicine in oncology, see for example Renfro and Mandrekar (2018). A first step in designing a clinical trial is to establish what is known about the disease being studied.
No comments:
Post a Comment